best Foot & Ankle treatment in chennai

Foot and Ankle
What is Plantar Fasciitis?
Plantar fasciitis refers to the inflammation of the plantar fascia, a thick band of tissue that is present at the bottom of the foot. It runs from the heel bone to the toes and forms the arch of your foot.
Plantar fasciitis is one of the most common causes of heel pain. It is most often seen in middle-aged men and women, but may also occur in those who are constantly on their feet.

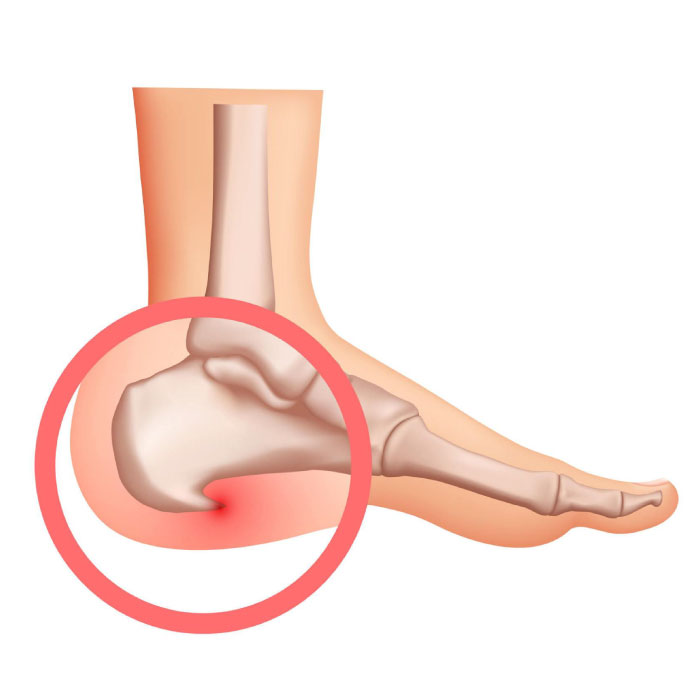
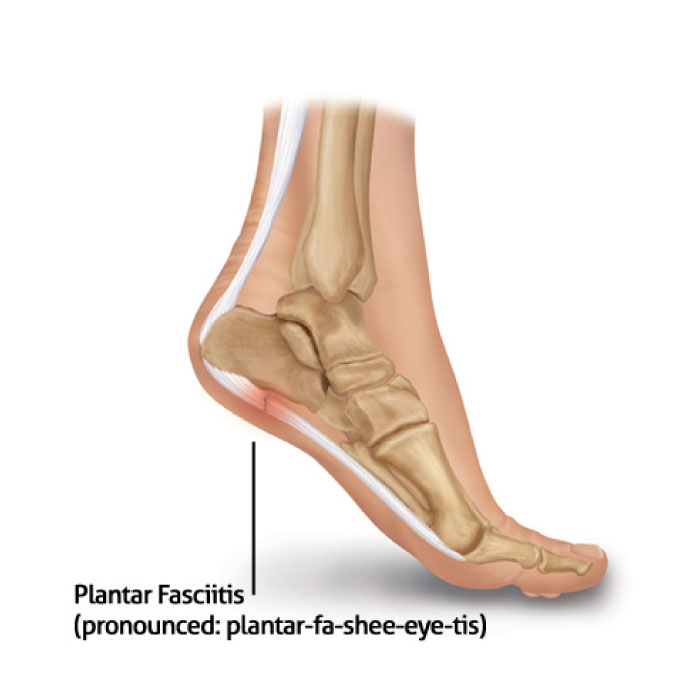
The plantar fascia functions as a shock absorber and supports the arch of your foot. Excessive pressure over the fascia may strain and tear the tissue, causing heel pain. Repeated overstretching or overuse causes irritation or inflammation of the fascia.
Other risk factors may include:
• Obesity
• Foot arch problems such as flat feet or high arches
• Activities such as long-distance running, ballet and dance aerobics
• Occupations that necessitate walking or standing on hard surfaces for a long period
• Wearing thin-soled shoes or shoes with poor arch support
The most common symptom is stabbing pain on the bottom of the foot, near the heel. You may experience pain when you take your first steps on awakening and it slowly decreases, but may return after standing for a long period of time.
Most often, you are effectively treated with the following measures:
• Medications: Your doctor may prescribe non-steroidal anti-inflammatory drugs (NSAIDs) or inject corticosteroids directly into the plantar fascia to reduce the pain and inflammation.
• Rest: Reduce or avoid the activities that worsen the pain.
• Ice: Apply ice packs over a towel on the painful area at least twice a day for 10 to 15 minutes for the first few days.
• Night splints: You may be prescribed night splints to stretch the plantar fascia and allow it to heal.
• Supportive shoes and orthotics: Your doctor may recommend shoes with good support and cushioning. Custom orthotics (shoe inserts) may also be helpful.
• Physical therapy: Your physical therapist may design an exercise program that focuses on stretching your plantar fascia and Achilles tendon, and strengthening the muscles of the lower leg. In addition to exercises, application of athletic tape to support the bottom of your foot may also help relieve symptoms.
• Extracorporeal shock wave therapy: During this procedure, sound waves are targeted on to the painful area to stimulate the healing process.
• Surgery: Occasionally, surgery may be suggested to release the tight plantar fascia.
Achilles Tendinitis
What is Achilles Tendinitis?
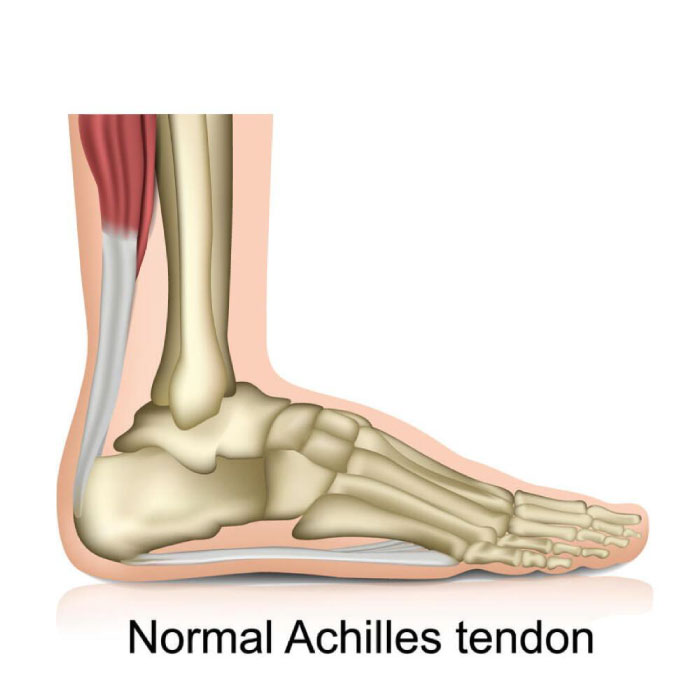
Inflammation of the Achilles tendon is known as Achilles tendinitis or tendonitis.
The Achilles tendon is a tough band of fibrous tissue that runs down the back of your lower leg and connects your calf muscle to your heel bone. The tendon is used when you walk, climb, jump, run and stand on your tip toes.
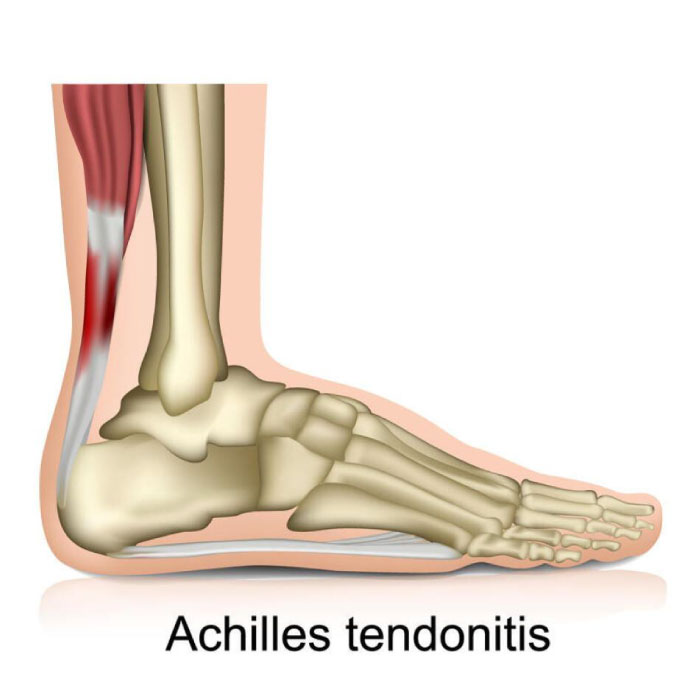
Achilles tendinitis occurs as a result of repetitive stress to the tendon. The stress may be due to:
• Overuse of the tendon
• Degeneration of the tendon
• Intense physical activity
• A sudden increase in activity
• Tight calf muscles
• Bone spurs or extra bone growth
• Rheumatoid arthritis and/or infection
Based on which part of the tendon is affected, Achilles tendinitis can be differentiated into:
• Insertional Achilles tendinitis: In this type, the lower portion of the tendon, where it attaches (inserts) to the heel bone is inflamed due to bone spurs.
• Non-insertional Achilles tendinitis: In this type, the middle portion of the tendon breaks down with tiny tears (degenerate), swells, and thickens. This is more commonly seen in younger and active people.
Some of the signs and symptoms of Achilles tendinitis include:
• Stiffness and pain along the Achilles tendon.
• Swelling and thickening of the tendon.
• Swelling or discomfort in the back of your heel.
• Pain in the back of your heel that worsens with activity.
• Tight and stiff calf muscle.
• The skin on the heel is warm to touch.
• Limited motion when you flex the foot.
If Achilles tendinitis is left untreated, it may cause:
• Severe pain
• Trouble walking or exercising
• Deformation of the tendon or heel bone
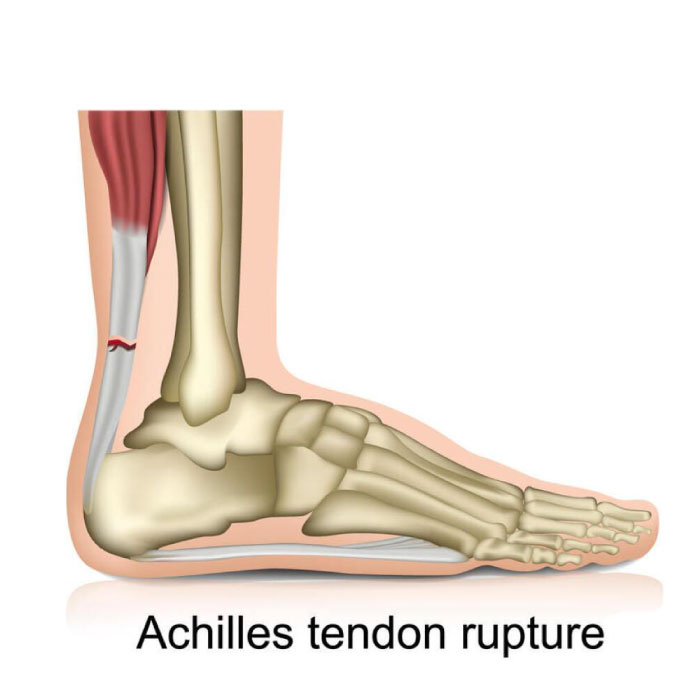
• Total tear or rupture of the Achilles tendon
To begin with, your doctor will physically examine your calf, heel, foot and ankle to look for symptoms associated with Achilles tendinitis and ask you some questions on how you got injured. Your doctor will also palpate the affected area to elucidate the exact location of pain or discomfort. Subsequently, imaging tests may be ordered to confirm the diagnosis of Achilles tendinitis. These tests include:
• X-rays: For images of leg bones and foot (to check for bone calcification)
• MRI scans: To detect tendon ruptures or tissue degeneration
• Ultrasounds: To check for tendon damage or inflammation
Treatment for Achilles tendonitis ranges from home remedies to nonoperative therapies to surgery.
As a home remedy, you may be advised to use RICE protocol: Rest, Ice, Compression (with bandage) and Elevation, which is usually effective in treating Achilles tendinitis.
Afterward, you may be given non-steroidal anti-inflammatory drugs (NSAIDs) or steroid or PRP injections as a nonoperative therapy. You may also be told to wear a brace and undergo physical therapy involving certain exercises.
If the pain does not improve after 6 months of nonsurgical treatment, surgery may be considered to repair your Achilles tendon. The specific type of surgery depends on the amount of damage to the tendon and the location of the tendinitis.
In an “open repair” type surgery, your surgeon:
• Makes a surgical cut above the heel bone to open your leg.
• Stitches the 2 sides of the ruptured tendon back together.
• Closes the incision to complete the surgery.
In another type of surgery, your surgeon:
• Makes a surgical cut to open the ruptured area of the leg.
• Passes needles with sutures through the tendon and the skin.
• Then ties the sutures together to complete the surgery.
Other surgical methods include:
• Debridement and repair: If the tendon has less than 50% damage, the damaged part is removed, and the remaining healthy part is repaired with sutures or stitches.
• Debridement with tendon transfer: In cases where the tendon has more than 50% damage and the remaining portion is not strong enough to function alone, an Achilles tendon transfer is performed.
• Gastrocnemius recession: This is the surgical lengthening of the calf muscles. The procedure is performed for people who have difficulty in flexing the foot, despite consistent stretching.
Though rare, complications such as infection, slow wound healing, damage to nerves and soft tissues, and bleeding may occur after any of the above surgeries. It may take you anywhere from a few weeks to a few months to recover fully.
Why choose iROS?
iROS Ortho Center is a multidisciplinary orthopedic center offering non-surgical and surgical treatment options including orthobiologics, physiotherapy or surgery to treat a wide range of joint pain indications.
- Expertise and Experience
- Patient-Centric Approach
- Simplifed Treatments
- Innovative Care

